Cardiovascular Pharmacotherapy Basics
Essential cardiovascular medications, mechanisms, clinical applications, and patient counseling for NAPLEX success.
Master cardiovascular pharmacotherapy with free flashcards and clinical scenarios that mirror real NAPLEX questions. This lesson covers hypertension management, heart failure medications, anticoagulation therapy, and lipid-lowering agents—essential concepts for passing the North American Pharmacist Licensure Examination and providing safe patient care.
Welcome to Cardiovascular Pharmacotherapy! 💊❤️
Cardiovascular disease remains the leading cause of death globally, making cardiovascular pharmacotherapy one of the most frequently tested areas on the NAPLEX. You won't just need to memorize drug names—you'll need to make clinical decisions about drug selection, dosing adjustments, monitoring parameters, and patient counseling.
This lesson focuses on the top cardiovascular medications you'll encounter in practice and on the exam. We'll emphasize clinical application over pure memorization, because NAPLEX tests your ability to think like a pharmacist, not just recall facts.
Core Concept 1: Hypertension Management 🩺
Hypertension affects nearly half of all adults in North America. The NAPLEX expects you to know first-line therapies, contraindications, and when to adjust treatment.
First-Line Antihypertensive Agents
| Drug Class | Example (Generic) | Mechanism | Key Monitoring |
|---|---|---|---|
| ACE Inhibitors | Lisinopril | Blocks conversion of angiotensin I → II | K+, SCr, dry cough |
| ARBs | Losartan | Blocks angiotensin II receptors | K+, SCr (no cough) |
| Calcium Channel Blockers | Amlodipine | Blocks Ca2+ entry → vasodilation | HR, edema, constipation |
| Thiazide Diuretics | Hydrochlorothiazide (HCTZ) | Blocks Na+ reabsorption in distal tubule | K+, Na+, glucose, uric acid |
Clinical Decision-Making: Drug Selection
💡 The NAPLEX loves asking WHY you'd choose one drug over another!
ACE Inhibitors/ARBs are preferred in patients with:
- Diabetes (renal protective)
- Heart failure (mortality benefit)
- Chronic kidney disease with proteinuria
⚠️ Contraindications:
- Pregnancy (Category D - causes fetal renal damage)
- Bilateral renal artery stenosis (can cause acute kidney injury)
- History of angioedema (ACE inhibitors only)
Calcium Channel Blockers are preferred in:
- African American patients (more effective than ACE/ARBs)
- Patients with bradycardia concerns (use dihydropyridines like amlodipine, NOT diltiazem/verapamil)
Thiazide Diuretics are:
- Cost-effective first-line for uncomplicated hypertension
- Less effective in patients with CrCl < 30 mL/min (switch to loop diuretics)
🧠 Memory Device: "ABCD of Hypertension"
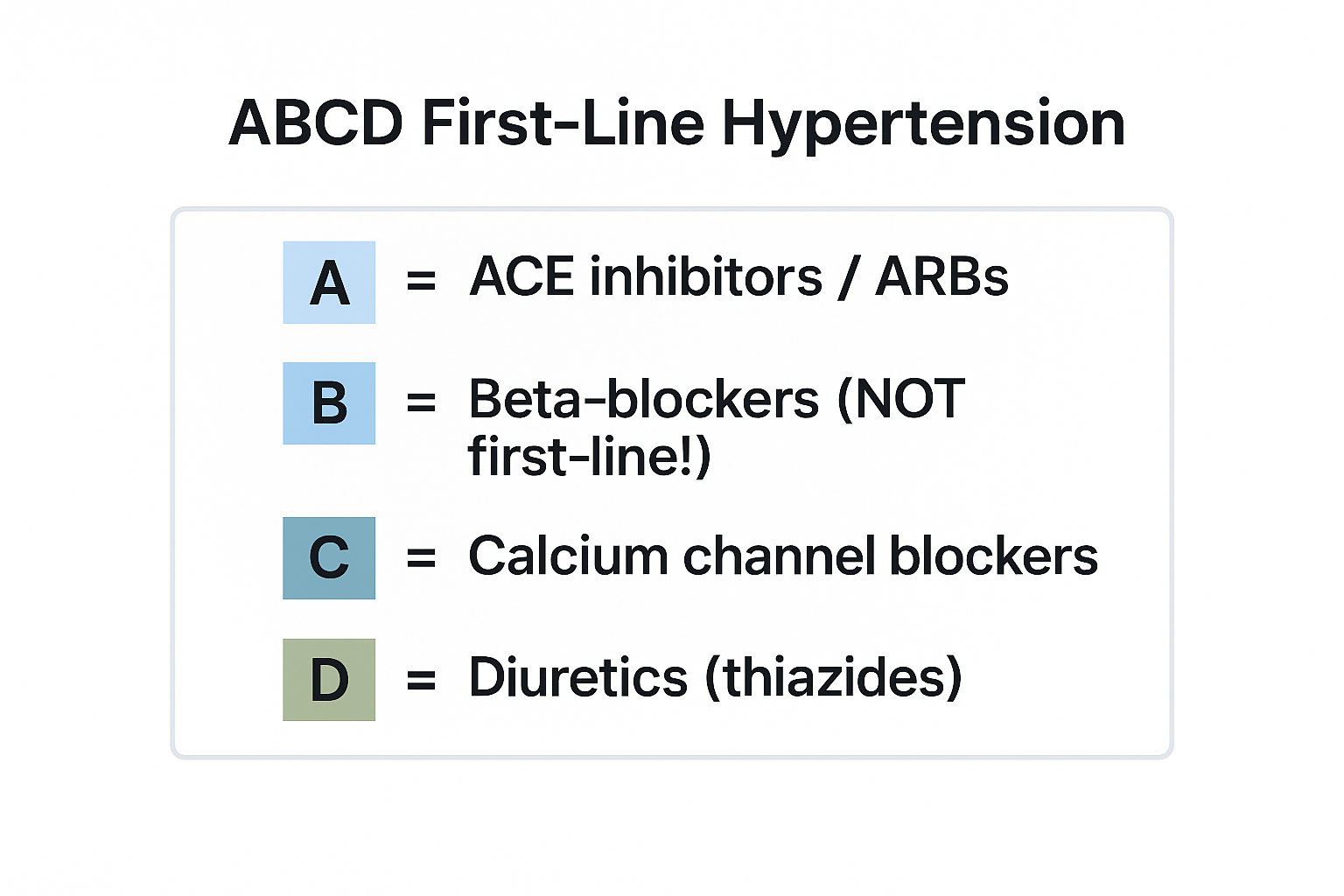
View original ASCII
┌─────────────────────────────────────┐ │ ABCD First-Line Hypertension │ ├─────────────────────────────────────┤ │ A = ACE inhibitors / ARBs │ │ B = Beta-blockers (NOT first-line!)│ │ C = Calcium channel blockers │ │ D = Diuretics (thiazides) │ └─────────────────────────────────────┘
Note: Beta-blockers are NOT first-line for uncomplicated hypertension anymore (per JNC guidelines) but are used for specific indications like heart failure or post-MI.
Core Concept 2: Heart Failure Pharmacotherapy 💔
Heart failure (HF) is classified as HFrEF (reduced ejection fraction, EF < 40%) or HFpEF (preserved ejection fraction, EF ≥ 50%). Drug selection differs dramatically!
HFrEF: Medications That Reduce Mortality
🎯 The "Fantastic Four" for HFrEF
| Drug Class | Example | Mortality Benefit |
|---|---|---|
| ACE/ARB/ARNI | Sacubitril/valsartan (Entresto) | ✅ Yes - reduces hospitalization |
| Beta-blockers | Carvedilol, metoprolol succinate | ✅ Yes - start LOW, go SLOW |
| MRAs | Spironolactone, eplerenone | ✅ Yes - monitor K+! |
| SGLT2 Inhibitors | Dapagliflozin, empagliflozin | ✅ Yes - newest addition! |
Key Clinical Pearls 💡
Sacubitril/valsartan (Entresto):
- ARNI = Angiotensin Receptor-Neprilysin Inhibitor
- More effective than ACE/ARB alone
- 36-hour washout required when switching from ACE inhibitor (prevents angioedema)
- Never combine with ACE inhibitors
Beta-blockers in HF:
- Only use carvedilol, metoprolol succinate (Toprol-XL), or bisoprolol
- NOT metoprolol tartrate (immediate-release)
- Start at low doses and titrate slowly (may worsen symptoms initially)
Mineralocorticoid Receptor Antagonists (MRAs):
- Spironolactone is non-selective (causes gynecomastia in men)
- Eplerenone is selective (fewer hormonal side effects)
- Monitor potassium and creatinine closely
- Avoid if K+ > 5.0 mEq/L or CrCl < 30 mL/min
Loop Diuretics (Furosemide):
- Used for symptom relief (reduce fluid overload)
- NO mortality benefit
- Dose based on renal function and fluid status
🔍 Clinical Scenario
Patient: 68-year-old male with HFrEF (EF 25%), currently on lisinopril 10 mg daily and furosemide 40 mg daily. BP 110/70, HR 82, K+ 4.2 mEq/L.
Question: What medication should be added next?
Answer: Beta-blocker (carvedilol or metoprolol succinate). Start with a low dose like carvedilol 3.125 mg BID and titrate up. The patient is already on an ACE inhibitor and diuretic, so guideline-directed medical therapy requires adding a beta-blocker next for mortality benefit.
Core Concept 3: Anticoagulation Therapy 🩸
Anticoagulation is high-risk - wrong dosing or drug interactions can cause life-threatening bleeding or clotting. NAPLEX will test monitoring, reversal agents, and drug interactions.
Warfarin vs. DOACs (Direct Oral Anticoagulants)
| Feature | Warfarin | DOACs (apixaban, rivaroxaban, dabigatran, edoxaban) |
|---|---|---|
| Monitoring | INR (target 2-3 for most indications) | No routine monitoring needed |
| Onset | Slow (3-5 days) - need heparin bridge | Fast (hours) |
| Reversal Agent | Vitamin K (slow), PCC/FFP (fast) | Idarucizumab (dabigatran), andexanet alfa (Xa inhibitors) |
| Food Interactions | Vitamin K foods (leafy greens) | Minimal |
| Renal Dosing | No adjustment | Required (especially dabigatran) |
| Cost | Inexpensive | Expensive |
Warfarin Drug Interactions (CRITICAL for NAPLEX!) ⚠️
Drugs that INCREASE INR (↑ bleeding risk):
- Antibiotics: Metronidazole, sulfamethoxazole/trimethoprim, fluoroquinolones
- Antifungals: Fluconazole, voriconazole
- Amiodarone (also decreases warfarin metabolism)
- NSAIDs (also increase bleeding via platelet inhibition)
Drugs that DECREASE INR (↓ anticoagulation):
- Rifampin (strong CYP inducer)
- Carbamazepine, phenytoin (enzyme inducers)
- Vitamin K supplements
🧠 Memory Device: "TICS" for Warfarin Interactions
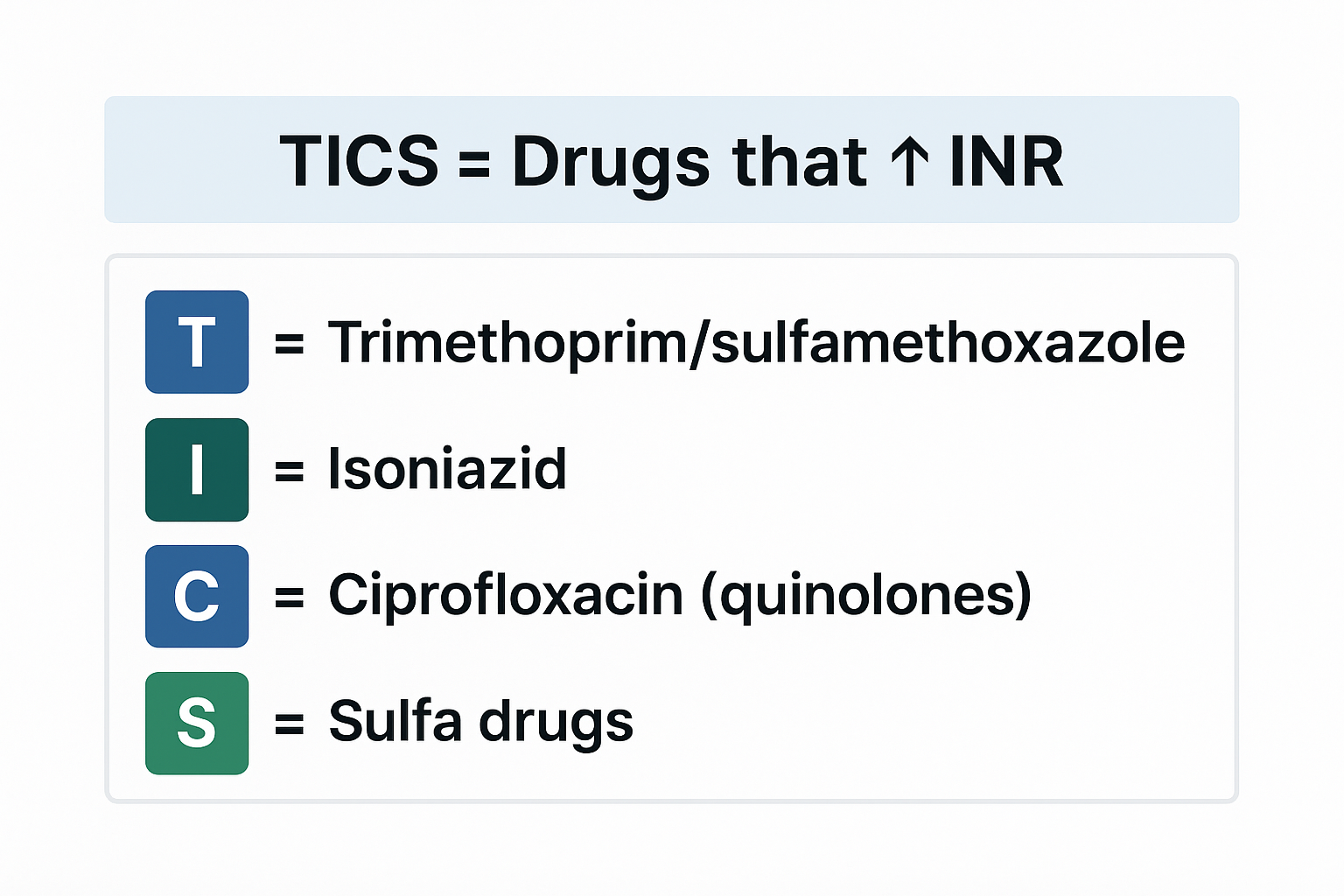
View original ASCII
┌────────────────────────────────────┐ │ TICS = Drugs that ↑ INR │ ├────────────────────────────────────┤ │ T = Trimethoprim/sulfamethoxazole │ │ I = Isoniazid │ │ C = Ciprofloxacin (quinolones) │ │ S = Sulfa drugs │ └────────────────────────────────────┘
DOAC Dosing in Atrial Fibrillation
Apixaban (Eliquis): 5 mg BID
- Reduce to 2.5 mg BID if patient has 2 of 3:
- Age ≥ 80 years
- Weight ≤ 60 kg
- SCr ≥ 1.5 mg/dL
Rivaroxaban (Xarelto): 20 mg daily with evening meal
- Reduce to 15 mg daily if CrCl 15-50 mL/min
Dabigatran (Pradaxa): 150 mg BID
- Reduce to 75 mg BID if CrCl 15-30 mL/min
- Contraindicated if CrCl < 15 mL/min
💡 Tip: DOACs require renal dose adjustments - always calculate CrCl using Cockcroft-Gault equation!
Core Concept 4: Lipid Management 📊
Statin therapy reduces cardiovascular events and mortality. NAPLEX focuses on statin intensity, monitoring, and adverse effects.
Statin Intensity Classification
| Intensity | LDL Reduction | Examples |
|---|---|---|
| High-Intensity | ≥ 50% | Atorvastatin 40-80 mg, Rosuvastatin 20-40 mg |
| Moderate-Intensity | 30-49% | Atorvastatin 10-20 mg, Simvastatin 20-40 mg, Rosuvastatin 5-10 mg |
| Low-Intensity | < 30% | Simvastatin 10 mg, Pravastatin 10-20 mg |
Who Gets High-Intensity Statins? 🎯
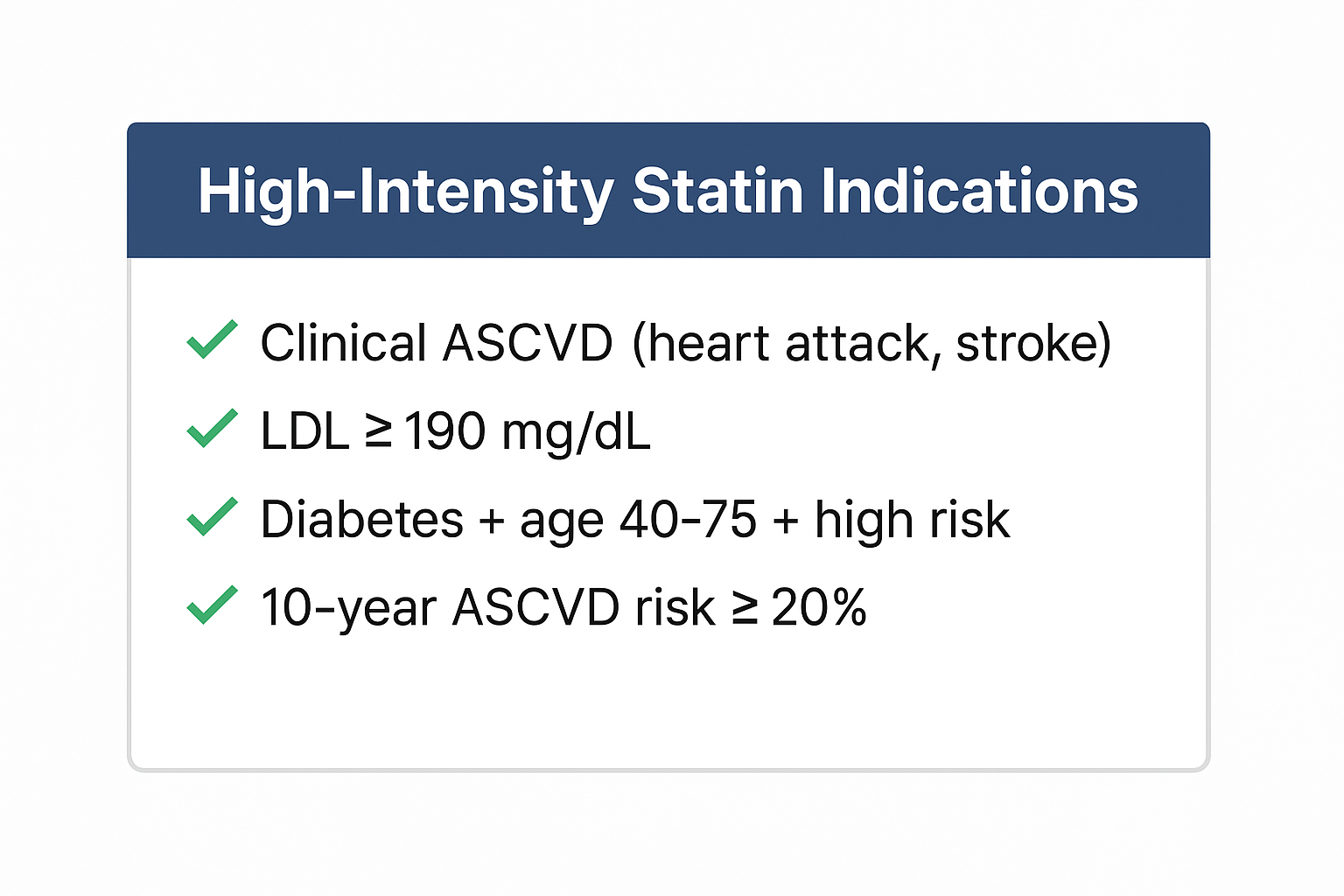
View original ASCII
┌──────────────────────────────────────────┐ │ High-Intensity Statin Indications │ ├──────────────────────────────────────────┤ │ ✓ Clinical ASCVD (heart attack, stroke) │ │ ✓ LDL ≥ 190 mg/dL │ │ ✓ Diabetes + age 40-75 + high risk │ │ ✓ 10-year ASCVD risk ≥ 20% │ └──────────────────────────────────────────┘
Statin Adverse Effects & Monitoring ⚠️
Myopathy/Rhabdomyolysis:
- Most serious adverse effect
- Symptoms: Muscle pain, weakness, dark urine
- Monitor CK (creatine kinase) if symptomatic
- Risk factors: High-dose statins, drug interactions, age > 80, hypothyroidism
Drug Interactions Increasing Myopathy Risk:
- Fibrates (especially gemfibrozil - avoid with statins!)
- Azole antifungals (itraconazole, ketoconazole)
- Macrolide antibiotics (clarithromycin, erythromycin)
- Grapefruit juice (inhibits CYP3A4 - affects atorvastatin, simvastatin, lovastatin)
Hepatotoxicity:
- Check baseline ALT/AST
- Recheck only if symptoms develop (no routine monitoring needed per guidelines)
- Discontinue if ALT/AST > 3× upper limit of normal
New-Onset Diabetes:
- Small increased risk (especially with high-intensity statins)
- Benefit of CV risk reduction outweighs diabetes risk - don't stop statin!
💊 Non-Statin Lipid Therapies
Ezetimibe (Zetia):
- Blocks cholesterol absorption in small intestine
- Reduces LDL by ~15-20%
- Add-on therapy when statin alone insufficient
- Minimal side effects
PCSK9 Inhibitors (Evolocumab, Alirocumab):
- Injectable monoclonal antibodies
- Reduce LDL by ~60%
- Very expensive - reserved for highest-risk patients
- Given every 2-4 weeks subcutaneously
Example Scenarios 🔍
Example 1: Hypertension with Comorbidities
Patient Profile:
- 55-year-old African American male
- BP: 158/96 mmHg (confirmed on multiple visits)
- Type 2 diabetes (A1C 7.2%)
- Creatinine: 1.1 mg/dL, CrCl: 75 mL/min
- No known drug allergies
Question: What is the BEST initial antihypertensive choice?
Answer: ACE inhibitor (e.g., lisinopril) or ARB (e.g., losartan)
Rationale: Despite being African American (where CCBs/thiazides are often more effective), the presence of diabetes makes ACE/ARBs the preferred choice due to their renal protective effects. They reduce proteinuria and slow progression of diabetic nephropathy. Combination therapy with a CCB or thiazide may be needed if BP goal not achieved.
Example 2: Warfarin Dosing Adjustment
Patient Profile:
- 72-year-old female on warfarin for atrial fibrillation
- Current dose: 5 mg daily
- INR results: Week 1 = 1.8, Week 2 = 1.9 (target INR 2-3)
- Started sulfamethoxazole/trimethoprim 3 days ago for UTI
Question: What action should you recommend?
Answer: Monitor INR more frequently; anticipate INR increase; may need to temporarily reduce warfarin dose
Rationale: Sulfamethoxazole/trimethoprim is a potent warfarin interaction that inhibits CYP2C9 and depletes vitamin K-producing gut bacteria. The patient's INR will likely increase significantly over the next week. Check INR in 3-5 days and consider reducing warfarin by 10-20% if INR rises above therapeutic range. Counsel patient on bleeding signs (bruising, blood in urine/stool, nosebleeds).
Example 3: Statin Selection
Patient Profile:
- 48-year-old male with recent MI (myocardial infarction)
- LDL: 145 mg/dL
- No muscle pain or weakness
- ALT/AST: Normal
- CrCl: 88 mL/min
Question: What statin regimen is most appropriate?
Answer: High-intensity statin: Atorvastatin 80 mg daily or Rosuvastatin 40 mg daily
Rationale: Patient has clinical ASCVD (MI), which is an absolute indication for high-intensity statin therapy regardless of LDL level. The goal is to reduce LDL by ≥50%. Atorvastatin 80 mg or rosuvastatin 40 mg are the only statins that consistently achieve this reduction. Moderate-intensity would be suboptimal for secondary prevention.
Example 4: Heart Failure Drug Initiation
Patient Profile:
- 65-year-old female with newly diagnosed HFrEF (EF 30%)
- BP: 132/84 mmHg, HR: 94 bpm
- Labs: Na+ 138, K+ 4.4, SCr 1.0, CrCl 72 mL/min
- Current meds: Furosemide 40 mg daily (started in hospital)
Question: What TWO medications should be initiated for mortality benefit?
Answer: ACE inhibitor (or ARB/ARNI) + Beta-blocker
Rationale: All patients with HFrEF should be started on guideline-directed medical therapy (GDMT) as soon as possible. The "Fantastic Four" are:
- ACE/ARB/ARNI
- Beta-blocker
- MRA (if K+ normal and adequate renal function)
- SGLT2 inhibitor
Start with ACE inhibitor (e.g., lisinopril 5 mg daily) and beta-blocker (e.g., carvedilol 3.125 mg BID). Titrate both to target doses. Add spironolactone 25 mg daily after ensuring K+ remains < 5.0. Add SGLT2 inhibitor (dapagliflozin 10 mg daily) for additional mortality benefit.
Common Mistakes to Avoid ⚠️
❌ Mistake 1: Using metoprolol tartrate for heart failure
Why it's wrong: Only metoprolol succinate (extended-release) has mortality benefit in HFrEF. Metoprolol tartrate (immediate-release) was not studied in heart failure trials.
❌ Mistake 2: Combining ACE inhibitor with sacubitril/valsartan
Why it's wrong: This combination dramatically increases angioedema risk. Always observe a 36-hour washout when switching from ACE to ARNI.
❌ Mistake 3: Not adjusting DOAC doses for renal function
Why it's wrong: DOACs (especially dabigatran) are renally eliminated. Failure to dose-adjust can cause accumulation and life-threatening bleeding. Always calculate CrCl using Cockcroft-Gault, not eGFR.
❌ Mistake 4: Stopping statins due to mild myalgia
Why it's wrong: Muscle aches are common (10-15% of patients) but rarely indicate serious myopathy. Check CK only if symptoms are severe or accompanied by weakness. Try different statin, lower dose, or alternate-day dosing before discontinuing entirely.
❌ Mistake 5: Forgetting vitamin K dietary counseling with warfarin
Why it's wrong: While patients don't need to avoid vitamin K foods, they should maintain consistent intake. Sudden increases in leafy greens can decrease INR; sudden decreases can increase bleeding risk.
❌ Mistake 6: Using thiazides in advanced CKD
Why it's wrong: Thiazide diuretics become ineffective when CrCl < 30 mL/min. Switch to loop diuretics (furosemide, bumetanide, torsemide) for patients with renal impairment.
Key Takeaways 🎯
📋 Quick Reference Card: Cardiovascular Pharmacotherapy
| Topic | Must-Know Points |
|---|---|
| Hypertension |
• First-line: ACE/ARB, CCB, thiazides • ACE/ARBs: Preferred for DM, HF, CKD with proteinuria • Contraindicated in pregnancy • Monitor K+, SCr |
| Heart Failure (HFrEF) |
• "Fantastic Four": ACE/ARB/ARNI + BB + MRA + SGLT2i • Use metoprolol succinate (NOT tartrate) • 36-hour washout: ACE → sacubitril/valsartan • Loop diuretics for symptoms only (no mortality benefit) |
| Anticoagulation |
• Warfarin: INR 2-3, monitor interactions • DOACs: Adjust for renal function • Dabigatran reversal: Idarucizumab • Xa inhibitor reversal: Andexanet alfa |
| Lipids |
• High-intensity statin for ASCVD, LDL ≥190, high-risk DM • Atorvastatin 40-80 mg or Rosuvastatin 20-40 mg • Monitor CK only if symptomatic myopathy • Avoid gemfibrozil + statin (↑myopathy risk) |
🔑 NAPLEX Success Tips:
• Always consider comorbidities when selecting therapy• Calculate renal function before dosing any medication
• Know drug interactions - especially warfarin, statins, DOACs
• Think about contraindications before selecting an answer
• Mortality benefit matters - know which drugs actually save lives vs. just treat symptoms
📚 Further Study
- ACC/AHA Hypertension Guidelines (2017): https://www.acc.org/guidelines/hypertension
- ACC/AHA Heart Failure Guidelines (2022): https://www.acc.org/guidelines/heart-failure
- Anticoagulation Dosing Guide - UpToDate: https://www.uptodate.com/contents/direct-oral-anticoagulants-dosing
Ready to test your knowledge? The following questions will challenge you to apply these concepts in realistic clinical scenarios—just like the NAPLEX! 💪