Safe and Effective Care Environment - Management of Care
Master essential management of care concepts for NCLEX-RN success, including client rights, delegation, ethical practice, and prioritization.
Master the fundamentals of safe and effective care management with free flashcards and structured practice. This lesson covers client rights, delegation and supervision, ethical and legal responsibilities, advance directives, informed consent, confidentiality, advocacy, interdisciplinary collaboration, case management, performance improvement, and prioritization—essential concepts for passing the NCLEX-RN examination and providing quality patient care.
Welcome to Management of Care! 👩⚕️
As a registered nurse, you'll make dozens of critical decisions every shift. Should you delegate this task to the nursing assistant? Does this patient understand the risks of their procedure? When multiple patients need care, who gets priority? These aren't just test questions—they're real scenarios you'll face daily.
The Management of Care category represents 17-23% of the NCLEX-RN exam and forms the foundation of safe, ethical nursing practice. Let's build your confidence in these essential skills.
Core Concepts in Management of Care 🎯
Client Rights and Advocacy 🛡️
Every patient has fundamental rights that nurses must protect and uphold. Understanding these rights isn't just about passing a test—it's about honoring human dignity.
Key Client Rights:
| Right | What It Means | Nursing Action |
|---|---|---|
| Autonomy | Self-determination in care decisions | Support patient choices even if you disagree |
| Confidentiality | Privacy of health information | Share information only with authorized personnel |
| Informed Consent | Understanding before agreeing to treatment | Ensure comprehension, not just a signature |
| Refusal of Treatment | Right to say "no" | Document refusal, notify provider, continue care |
| Safe Environment | Freedom from harm or abuse | Implement safety measures, report concerns |
Advocacy means speaking up for patients who cannot speak for themselves or need support navigating the healthcare system. You're the patient's voice!
💡 Pro Tip: When a patient's family says "Don't tell Dad about his cancer diagnosis," remember: The patient has the right to their own health information. You must advocate for the patient's autonomy, not the family's preference.
🔍 Real-World Scenario: Mrs. Chen, 78, is scheduled for surgery tomorrow morning. Her daughter signed the consent form because "Mom doesn't understand medical things." As her nurse, you must:
- Verify Mrs. Chen can understand the procedure herself
- Use an interpreter if there's a language barrier
- Ensure SHE consents, not just her daughter
- Document her level of understanding
If Mrs. Chen cannot understand due to cognitive impairment, the daughter would need legal authority (healthcare proxy/power of attorney) to consent on her behalf.
Informed Consent ✍️
Informed consent is MORE than a signature—it's a process ensuring the patient truly understands what they're agreeing to.
Three Essential Elements:
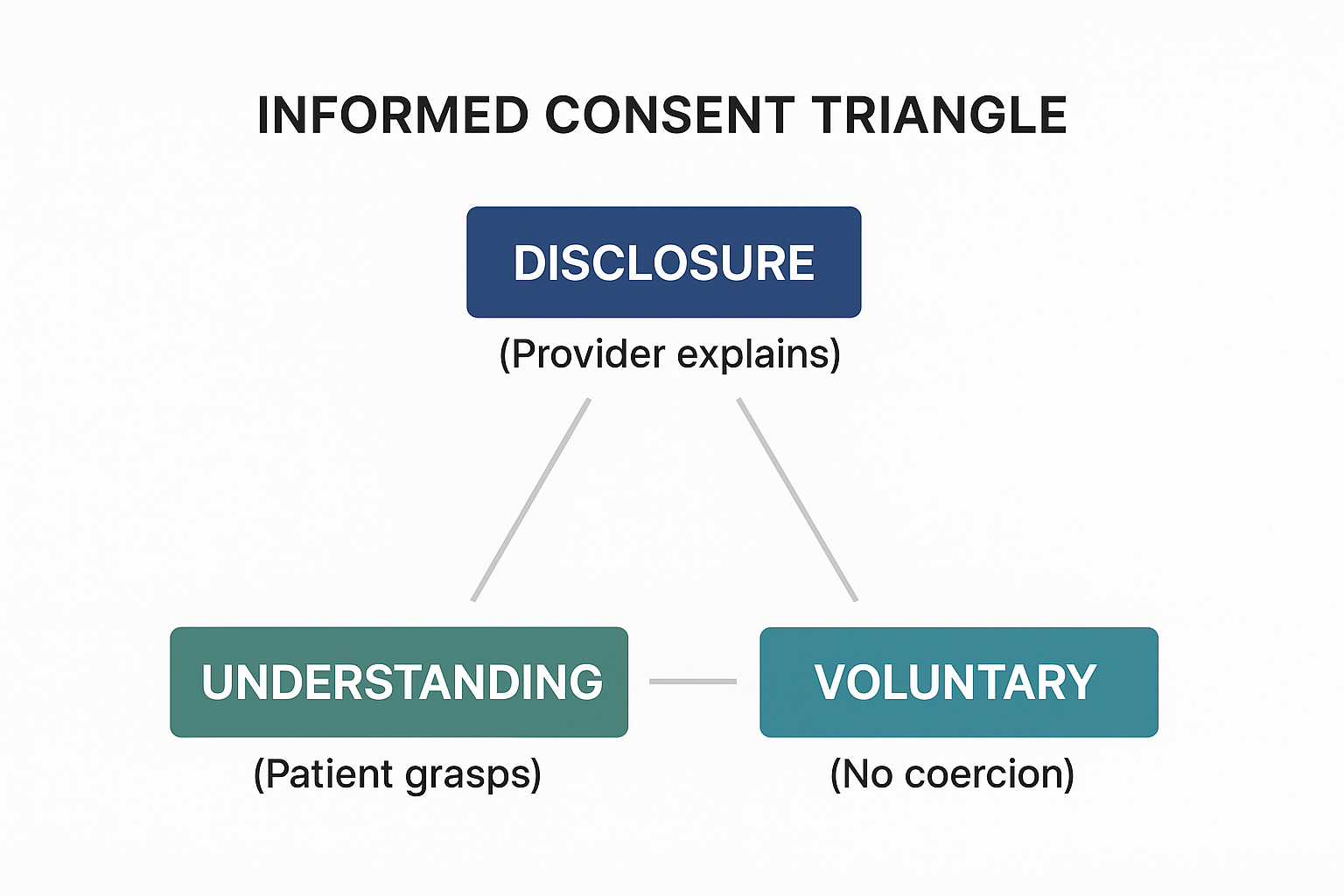
View original ASCII
┌─────────────────────────────────────────┐ │ INFORMED CONSENT TRIANGLE │ │ │ │ 📋 DISCLOSURE │ │ (Provider explains) │ │ /\ │ │ / \ │ │ / \ │ │ / \ │ │ / \ │ │ / \ │ │ 🧠 UNDERSTANDING ✅ VOLUNTARY │ │ (Patient grasps) (No coercion) │ │ │ └─────────────────────────────────────────┘
What Must Be Disclosed:
- Nature of the procedure/treatment
- Risks and benefits
- Alternative options (including doing nothing)
- Expected outcomes
The Nurse's Role vs. The Provider's Role:
| Provider Responsibility | Nurse Responsibility |
|---|---|
| Explain the procedure, risks, benefits | Witness the signature |
| Answer medical questions | Verify patient understanding |
| Obtain the consent | Ensure voluntariness (no pressure) |
| Document the discussion | Notify provider if patient has questions |
⚠️ Common Mistake: Nurses cannot obtain informed consent for medical procedures—only physicians/providers can. You can witness the signature AFTER the provider has explained everything.
💡 Red Flags - Stop and Notify Provider:
- Patient says "I'm still not sure what they're doing"
- Patient asks medical questions you can't answer
- Patient appears confused or sedated
- Patient says "My family really wants me to do this"
- Patient is a minor without parent/guardian present
Special Situations:
- Emergencies: Implied consent when patient cannot consent and treatment is life-saving
- Minors: Parent/guardian must consent (exceptions: emancipated minors, emergencies)
- Incompetent Adults: Legal healthcare proxy or court-appointed guardian consents
Advance Directives 📜
Advance directives are legal documents expressing healthcare wishes if the patient becomes unable to communicate. Think of them as "future instructions."
Two Main Types:
📋 Advance Directive Quick Reference
| Type | Purpose | Example |
|---|---|---|
| Living Will | States treatment preferences | "No CPR if terminally ill" |
| Durable Power of Attorney for Healthcare | Names decision-maker | "My sister decides for me" |
Do Not Resuscitate (DNR) Orders:
- A physician order based on patient wishes
- Means no CPR if heart/breathing stops
- Does NOT mean "do not treat"—all other care continues
- Must be in the medical record
Your Nursing Responsibilities:
- Ask on admission if patient has advance directives
- Place copies in the medical record
- Ensure all team members know about them
- Honor the directives even if you personally disagree
- Support the patient's designated decision-maker
🤔 Did You Know? Only about 30% of Americans have advance directives, yet most believe these discussions are important. As a nurse, you can encourage patients to complete them while they're healthy and clear-headed.
Delegation and Supervision 👥
Delegation is transferring responsibility for a task while retaining accountability for the outcome. You're still responsible even when someone else does the work!
The Five Rights of Delegation:

View original ASCII
┌────────────────────────────────────────┐ │ THE 5 RIGHTS OF DELEGATION │ ├────────────────────────────────────────┤ │ │ │ 1️⃣ RIGHT TASK │ │ (Can this be delegated?) │ │ ↓ │ │ 2️⃣ RIGHT PERSON │ │ (Do they have the skills?) │ │ ↓ │ │ 3️⃣ RIGHT CIRCUMSTANCES │ │ (Is the patient stable?) │ │ ↓ │ │ 4️⃣ RIGHT DIRECTION │ │ (Clear, specific instructions) │ │ ↓ │ │ 5️⃣ RIGHT SUPERVISION │ │ (Monitor and evaluate) │ │ │ └────────────────────────────────────────┘
What Can You Delegate?
| Healthcare Role | CAN Delegate | CANNOT Delegate |
|---|---|---|
| UAP/Nursing Assistant | ADLs (bathing, feeding, toileting) Vital signs on stable patients Ambulation Bed making | Assessment Medication administration Sterile procedures Patient teaching Care planning |
| LPN/LVN | Basic care Data collection Some medications (varies by state) Dressing changes | Initial assessment IV push meds (most states) Patient education requiring RN judgment |
💡 Memory Device - "ADELE Never Teaches Patients"
- Assessment
- Decision-making
- Evaluation
- Learning (patient teaching)
- Expert nursing judgment
These CANNOT be delegated—they're RN responsibilities!
⚠️ Delegation Danger Zone: NEVER delegate assessment, teaching, or evaluation. Even if an LPN has 20 years of experience, initial patient assessment is YOUR job as the RN. You can delegate data collection ("Take Mr. Smith's blood pressure"), but not assessment ("Is Mr. Smith's cardiovascular status stable?").
Proper Delegation Communication:
❌ Vague: "Can you check on the patient in 202?"
✅ Clear: "Please measure Mrs. Johnson's blood pressure in room 202 at 2 PM. She's stable post-op day 1. Call me immediately if it's below 100 systolic or if she reports dizziness. I'll come evaluate her at 2:30 PM."
Notice the specific task, clear parameters, and follow-up plan!
Confidentiality and HIPAA 🔒
The Health Insurance Portability and Accountability Act (HIPAA) protects patient privacy. Violations can result in fines, job loss, and even criminal charges.
Protected Health Information (PHI) includes:
- Name, address, birth date
- Medical record number
- Diagnoses and treatments
- Test results
- Photos of patients
- Even the FACT that someone is your patient
When Can You Share Information?
| Situation | Can Share? | Why? |
|---|---|---|
| With the healthcare team caring for patient | ✅ YES | "Need to know" for treatment |
| With patient's family | ⚠️ ONLY with patient permission | Patient controls who knows |
| With your spouse at dinner | ❌ NO | Not involved in care |
| Court order/subpoena | ✅ YES | Legal requirement |
| Suspected abuse | ✅ YES | Mandatory reporting |
| Communicable disease to health department | ✅ YES | Public health requirement |
⚠️ HIPAA Violations to Avoid:
- Discussing patients in elevators, cafeteria, or public areas
- Accessing medical records of patients not assigned to you
- Posting about patients on social media (even without names!)
- Leaving patient charts open where others can see
- Giving information to "the patient's friend" without verification
💡 The Grocery Store Test: If you see your patient at the grocery store, don't acknowledge you know them first—they may not want to be identified as a patient. Let them approach you.
Prioritization and Time Management ⏰
In nursing, everything seems urgent—but you can only be in one place at a time. Prioritization keeps patients safe.
Prioritization Frameworks:
1. Maslow's Hierarchy (Physiological Needs First):
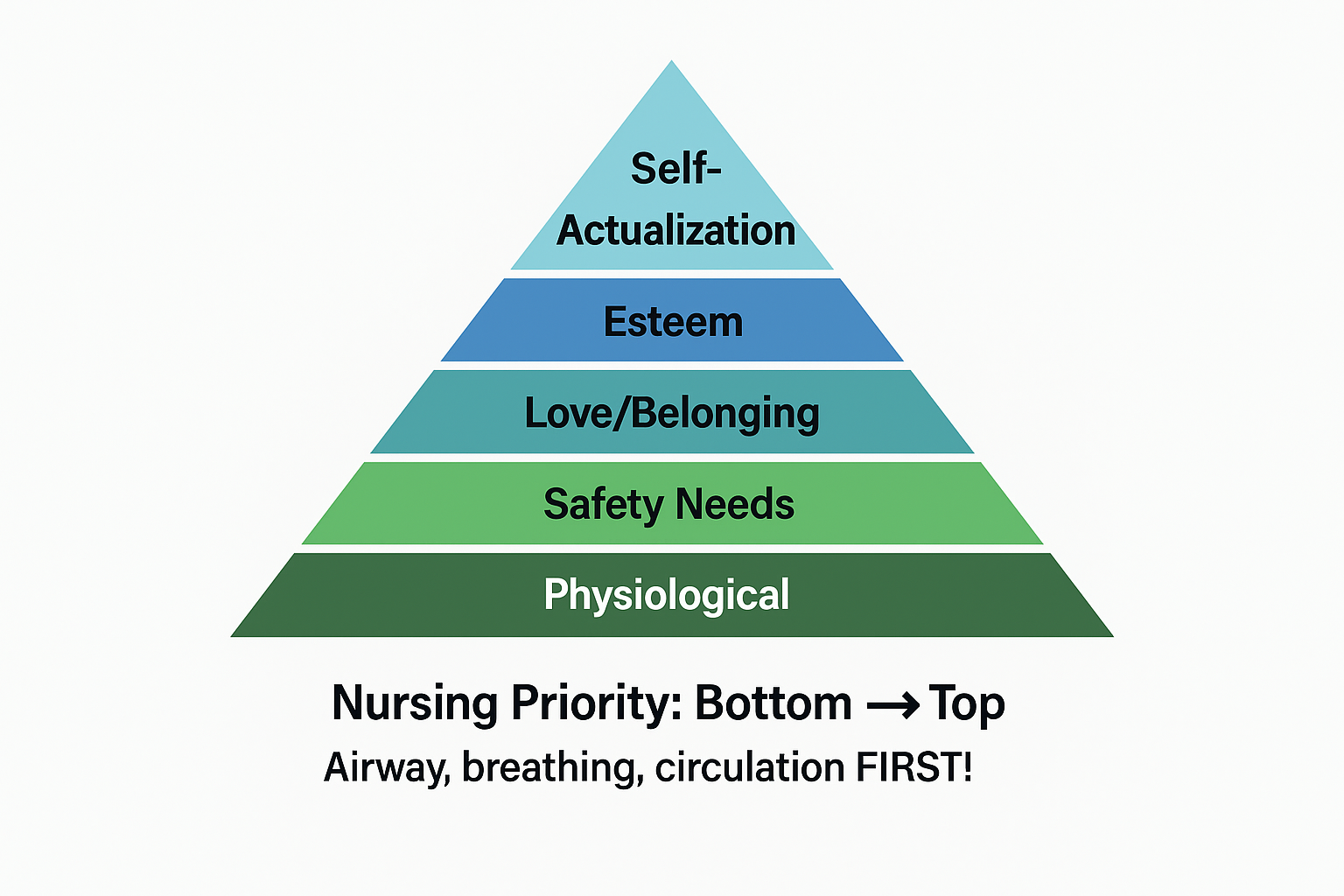
View original ASCII
/\
/🎯\
/ Self \
/Actualization\
/──────────────\
/ 🏆 Esteem \
/──────────────────\
/ 💕 Love/Belonging \
/────────────────────────\
/ 🔒 Safety Needs \
/────────────────────────────\
/ 🍞 Physiological \
────────────────────────────────
Nursing Priority: Bottom → Top
Airway, breathing, circulation FIRST!
2. ABC Priority (Life-Threatening First):
- Airway (Is it open? Obstructed?)
- Breathing (Are they breathing adequately?)
- Circulation (Is their heart pumping? Are they bleeding?)
3. Acute vs. Chronic:
- Acute, sudden changes → Higher priority
- Chronic, stable conditions → Lower priority
4. Actual vs. Potential Problems:
- Actual problems (happening now) → Higher priority
- Risk for problems (might happen) → Lower priority
Priority Decision-Making Examples:
🚨 Prioritization Scenarios
Scenario 1: Four patients need you NOW
- Patient A: Requesting pain medication (7/10 pain)
- Patient B: Call light on - needs to use bathroom
- Patient C: Oxygen saturation alarm - reading 88%
- Patient D: Family member wants to speak with you
Priority Order: C → B → A → D
Why?
- C first: Low oxygen (88%) is life-threatening - ABC priority
- B second: Fall risk if patient attempts to get up alone - safety issue
- A third: Pain is important but not immediately life-threatening
- D last: Can wait; no immediate patient care need
💡 The "Will They Die?" Test: When prioritizing, ask yourself: "If I delay this 5 minutes, could the patient suffer serious harm or death?" If yes, it's your top priority.
Unstable Before Stable Rule:
- Post-op patient with dropping blood pressure → See BEFORE
- Patient admitted 3 days ago, stable, requesting magazines → See AFTER
Ethical Practice ⚖️
Ethics guide your decisions when there's no clear "right" answer. Nursing ethics are built on core principles.
Four Ethical Principles:
| Principle | Definition | Nursing Example |
|---|---|---|
| Autonomy | Respect for self-determination | Supporting a patient's refusal of treatment even if you disagree |
| Beneficence | Doing good for the patient | Providing comfort measures during a painful procedure |
| Nonmaleficence | Preventing harm ("first, do no harm") | Questioning an order that seems unsafe |
| Justice | Fairness in care distribution | Providing equal care regardless of patient's ability to pay |
Ethical Dilemmas You'll Face:
🔍 Scenario: A patient with terminal cancer wants to continue aggressive treatment. The family wants to "let her go peacefully." The medical team thinks treatment is futile.
Ethical Analysis:
- Autonomy: Patient's right to choose
- Beneficence vs. Nonmaleficence: Treatment might extend life (good) but cause suffering (harm)
- Justice: Healthcare resources
Your Role: Advocate for the PATIENT'S wishes, facilitate communication between all parties, support whatever decision is made.
⚠️ Ethical vs. Legal: Sometimes what's legal isn't ethical, and vice versa. Ethics are moral principles; laws are rules. You must follow laws, but you can advocate for ethical changes.
Collaboration with the Interdisciplinary Team 🤝
Healthcare is a team sport! Effective collaboration improves patient outcomes.
Key Team Members:
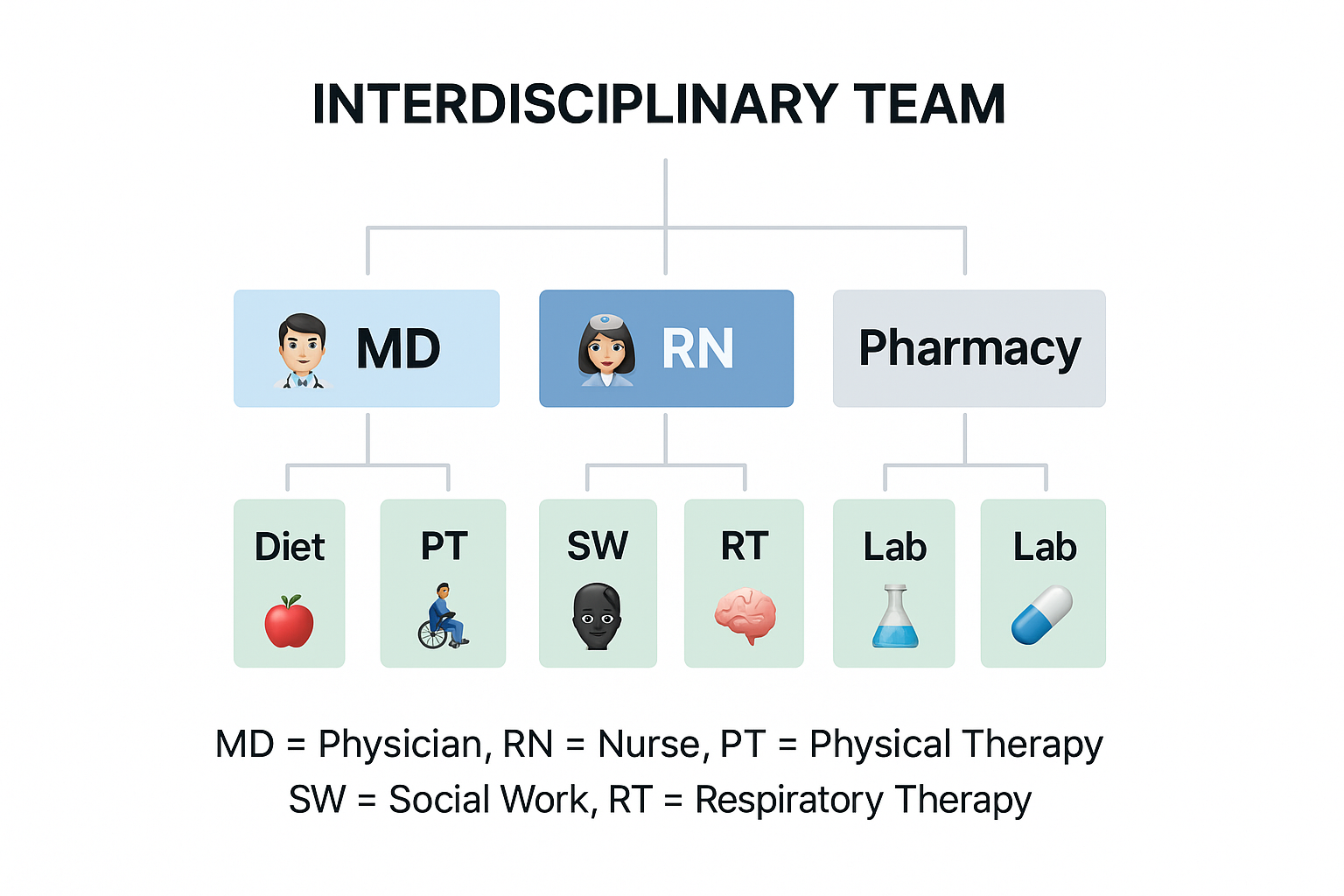
View original ASCII
INTERDISCIPLINARY TEAM
│
┌─────────┼─────────┐
│ │ │
👨⚕️ MD 👩⚕️ RN 💊 Pharmacy
│ │ │
┌───┴───┐ ┌───┴───┐ ┌───┴───┐
│ │ │ │ │ │
🍎 Diet 🧑🦽 PT 🧠 SW 👨⚔️ RT 🧪 Lab
MD = Physician, RN = Nurse, PT = Physical Therapy
SW = Social Work, RT = Respiratory Therapy
Communication Tools:
SBAR: The Universal Healthcare Language
| Component | What to Say | Example |
|---|---|---|
| Situation | What's happening RIGHT NOW | "Mr. Lee's blood pressure is 82/50" |
| Background | Relevant patient history | "He's post-op day 1 hip replacement, normally BP 130/80" |
| Assessment | What you think is going on | "I'm concerned about possible internal bleeding" |
| Recommendation | What you want to happen | "Can you come assess him now?" |
💡 Pro Tip: SBAR keeps communication focused and complete. Use it when calling physicians, giving report, or requesting consultations.
Case Management and Referrals:
Case managers coordinate care across the continuum—from hospital to home. Your role:
- Identify patients needing case management (complex care, multiple comorbidities, discharge barriers)
- Provide referrals to appropriate services (home health, physical therapy, social services)
- Communicate patient needs clearly
Detailed Examples 📚
Example 1: Delegation Decision
Scenario: You're caring for four patients. The nursing assistant asks for an assignment. What can you delegate?
Patients:
- Mr. Adams - stable, needs vital signs and morning bath
- Mrs. Baker - new admission, needs initial assessment
- Mr. Chen - diabetic, needs blood glucose check before lunch
- Mrs. Davis - post-op, needs IV pain medication
Analysis:
| Task | Can Delegate to UAP? | Rationale |
|---|---|---|
| Mr. Adams - vital signs and bath | ✅ YES | Stable patient, routine ADLs and vital signs |
| Mrs. Baker - initial assessment | ❌ NO | Assessment requires RN judgment |
| Mr. Chen - blood glucose check | ✅ YES (in most facilities) | Stable patient, routine monitoring. UAP trained in glucose testing |
| Mrs. Davis - IV pain medication | ❌ NO | Medication administration requires RN license |
What You Delegate: "Please take Mr. Adams' vital signs at 9 AM and help him with his bath. Also check Mr. Chen's blood glucose at 11:30 AM before lunch. Call me if his vitals are outside normal limits or his glucose is below 70 or above 250. I'll be assessing Mrs. Baker and giving Mrs. Davis her pain medication."
Follow-up: At 10 AM, you check with the nursing assistant about completion status and any findings.
Example 2: Prioritization Challenge
Scenario: You've just received morning report on your four patients. Where do you start?
Report:
- Room 101: 45-year-old admitted last night with chest pain, currently pain-free, scheduled for stress test today
- Room 102: 68-year-old post-op day 2 hip replacement, vital signs stable, requesting pain medication
- Room 103: 82-year-old with pneumonia, oxygen saturation 91% on 2L oxygen, respiratory rate 24
- Room 104: 55-year-old with diabetes, blood glucose this morning was 350, insulin ordered
Decision Process:
| Patient | Priority Level | Rationale |
|---|---|---|
| Room 103 | 🔴 HIGHEST | ABC priority - breathing issue, elderly with infection |
| Room 104 | 🟡 HIGH | Very high glucose could lead to DKA if untreated |
| Room 102 | 🟢 MODERATE | Stable post-op, pain managed |
| Room 101 | 🔵 LOWER | Currently stable, pain-free |
Your Action Plan:
- First (5 minutes): Room 103 - Assess respiratory status, lung sounds, consider need for increased oxygen or provider notification
- Second (10 minutes): Room 104 - Administer insulin, assess for DKA symptoms
- Third (15 minutes): Room 102 - Assess pain level, administer pain medication
- Fourth (20 minutes): Room 101 - Routine assessment, prepare for stress test
Example 3: Ethical Dilemma
Scenario: Mrs. Thompson, 72, has advanced dementia. She frequently pulls out her IV lines. The physician suggests soft wrist restraints. The family agrees. Mrs. Thompson becomes agitated when you approach with restraints.
Ethical Analysis:
Competing Principles:
- Nonmaleficence: Restraints might prevent her from pulling IVs and causing harm
- Autonomy: She's resisting (even without capacity to verbally refuse)
- Beneficence: She needs the IV fluids and medications
Alternative Solutions to Explore FIRST:
- Could a PICC line (harder to pull) replace peripheral IV?
- Can family member stay with her to redirect behaviors?
- Can IV fluids be given at night while she sleeps?
- Would mittens (less restrictive) prevent pulling?
- Is the IV absolutely necessary, or can medications be given another way?
Restraint Rules:
- Use ONLY as last resort
- Must have physician order
- Requires frequent monitoring (every 15-30 minutes)
- Must release every 2 hours for movement
- Document behavior necessitating restraints
- Reassess need frequently
Your Advocacy Role: Present alternatives to the physician and family. If restraints are deemed necessary, ensure they're used correctly with proper monitoring.
Example 4: Confidentiality Situation
Scenario: You're caring for State Senator Rodriguez, admitted for pneumonia. A reporter calls the unit asking about his condition. The senator's adult son approaches you in the hallway asking for an update "before he goes into Dad's room."
Analysis:
Reporter on the phone:
- ❌ CANNOT confirm patient is even on your unit
- ❌ CANNOT provide any information
- ✅ CAN say "I cannot confirm or deny any patient information without authorization"
- ✅ CAN direct them to hospital public relations if patient has authorized a spokesperson
Senator's son in hallway:
- ❌ CANNOT discuss in public hallway (others might hear)
- ⚠️ CANNOT automatically assume family has permission
- ✅ MUST verify patient has authorized information sharing with son
- ✅ SHOULD invite son into private area or patient's room for discussion
Proper Response to Son: "I'm glad you're here to visit. Let's step into your father's room where we can talk privately. I'll need to confirm with him that it's okay to discuss his care with you." (This respects confidentiality while being family-friendly.)
If Senator is Unconscious: Check chart for documented healthcare proxy. If son is the proxy, you can share information. If not documented, verify identity and relationship, but limit details until authorization is confirmed.
Common Mistakes to Avoid ⚠️
Mistake #1: Delegating What You Shouldn't
❌ Wrong: "Can you teach Mr. Jones how to use his insulin pen?"
Patient teaching requires RN assessment of learning needs, comprehension, and evaluation—cannot be delegated to UAP.
✅ Right: "Please remind Mr. Jones to press his call light when the diabetes educator arrives at 2 PM."
Mistake #2: Signing Consent Forms You Shouldn't
❌ Wrong: Patient asks what the surgery involves, you explain it, they sign the consent, you witness it.
You've just performed the physician's job! You can only witness consent AFTER the physician has explained everything.
✅ Right: "Let me call Dr. Smith to come answer your questions before you sign anything."
Mistake #3: Prioritizing by Who Yells Loudest
❌ Wrong: Family member is demanding you come NOW, so you leave a patient with low oxygen to address their complaint about cold food.
✅ Right: "I understand your concern about the food. I need to attend to another patient's breathing right now, but I'll have someone from dietary come speak with you within 10 minutes."
Mistake #4: Discussing Patients in Public
❌ Wrong: Texting your nursing friend: "OMG, you won't believe what happened with my patient in room 405!"
Even without names, specific details (room number) identify patients. This violates HIPAA.
✅ Right: Vent about stressful days in general terms: "Today was rough, three admissions and a code!" (No identifying details.)
Mistake #5: Putting Family Wishes Above Patient Rights
❌ Wrong: Adult daughter says "Don't tell Mom about her cancer diagnosis," and you comply.
Competent adult patients have the RIGHT to their own health information.
✅ Right: "Your mother has the right to know about her diagnosis. Let's talk with her together about how she wants to receive information. Some patients prefer family members present, others want privacy."
Mistake #6: Ignoring Advance Directives Because Family Disagrees
❌ Wrong: Patient has DNR, but family says "Do everything!" so you initiate CPR.
The patient's documented wishes override family preferences (unless family is the legal healthcare proxy and patient is now incompetent).
✅ Right: Follow the DNR. Explain to family: "I know this is difficult, but I must honor your loved one's wishes as documented. Let's focus on keeping them comfortable."
Key Takeaways 🎯
📋 Management of Care - Quick Reference Card
CLIENT RIGHTS (CRASP):
- Confidentiality - Protect their privacy
- Refuse treatment - They can say no
- Autonomy - Self-determination in decisions
- Safe environment - Freedom from harm
- Privacy - Dignity and respect
INFORMED CONSENT - Three Must-Haves:
- ✅ Disclosure (provider explains risks/benefits)
- ✅ Understanding (patient comprehends)
- ✅ Voluntary (no coercion)
CANNOT DELEGATE (ADELE):
- Assessment
- Decision-making
- Evaluation
- Learning (patient teaching)
- Expert nursing judgment
PRIORITIZATION:
- 🔴 ABC - Airway, Breathing, Circulation (always first!)
- 🟡 Acute before Chronic
- 🟢 Unstable before Stable
- 🔵 Actual problems before Potential problems
ETHICAL PRINCIPLES (ABJN):
- Autonomy - Respect patient choices
- Beneficence - Do good
- Justice - Be fair
- Nonmaleficence - Prevent harm
COMMUNICATION WITH TEAM (SBAR):
- Situation - What's happening now
- Background - Relevant history
- Assessment - What you think
- Recommendation - What you want
HIPAA - When Can You Share?
- ✅ Healthcare team caring for patient
- ✅ With patient permission
- ✅ Court order or mandatory reporting (abuse)
- ❌ Family without permission
- ❌ Friends, your family, social media
📚 Further Study
For additional preparation and deeper understanding of Management of Care concepts:
American Nurses Association - Code of Ethics: https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/
National Council of State Boards of Nursing (NCSBN) - Delegation Resources: https://www.ncsbn.org/public-files/delegation.pdf
U.S. Department of Health & Human Services - HIPAA for Professionals: https://www.hhs.gov/hipaa/for-professionals/index.html
💪 You're building the foundation of safe, ethical nursing practice! These concepts aren't just test material—they're the principles that will guide your daily decisions as an RN. Review the flashcards, practice prioritization scenarios, and remember: when in doubt, advocate for your patient's rights and safety. You've got this! 🌟